In today’s fast-paced world, a large section of the population is denied the opportunity to manage chronic diseases through a wellness, holistic and healing-oriented approach.
Dr. Ennapadam S Krishnamoorthy
The burden of chronic disorders is largely attributed to the perils of modern medicine that prioritises cure through prescription drugs instead of focusing on the entire continuum of human healthcare engagement: rejuvenation, restoration and rehabilitation. The end result: an unhealthy ageing population.This is where India’s ancient and holistic Ayurvedic system as a viable form of alternative medicine comes in. It is about time medical practitioners harnessed the full potential of Ayurveda as it’s based on a strong foundation of scientific research, much like modern medicine’s tenets.
In recent years, a growing body of research points to integrated medical treatments—a combination of complementary (alternative) and modern (allopathic) medicine—gaining popularity. While modern medicine’s thrust is on cure, integrative medicine focuses on disease prevention, comfort and care.
However, despite the marked shift in patients’ preference for alternative forms of healing, I observed a deficit of innovation in therapies that are based on integrative medicine. This is where Buddhi Clinic’s genesis and my entrepreneurial journey can be traced.
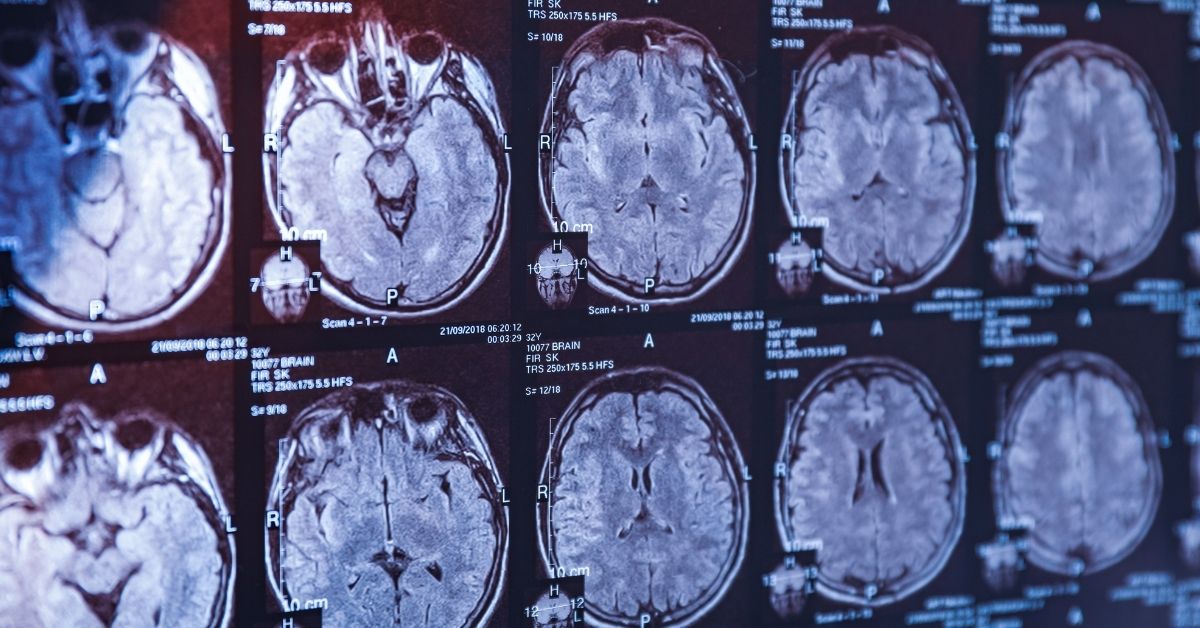
I realised there was no other healthcare outfit in the world that provides a unique 360° evaluation of body, brain and mind through an integrated approach. At Buddhi, we take a holistic approach to diagnose a medical condition that combines the scientific rigour of modern medicine’s diagnosis and drug treatments with the therapeutic benefits of ancient healing traditions.
In essence, my long-term vision for our healthcare startup that was founded as a project in 2009 and company in 2013, is to make complementary and alternative medicine (CAM) gain acceptance as mainstream therapies. From my experience, I realised this would be possible only by seamlessly integrating them with modern medicine.
Let me tell you how this is done at Buddhi Clinic.
A Game-Changer in Brain and Mind Integrated Therapy
We are the pioneers and innovators of integrated care for the brain and mind. What sets Buddhi Clinic apart from the rest is that we don’t follow a cookie-cutter approach to diagnosis and treatment. Our raison d’être lies in being able to provide unique personalised treatment strategies for patients that is managed by interdisciplinary process-driven programmes.
Since several neurological and mental health disorders and disability are longstanding issues, patients need continuous and comprehensive care. Thus, we strive to offer a better quality of daily life to our patients by curating a range of therapeutic solutions based on considerable clinical and empirical research, and our team’s extensive experience.
Buddhi Clinic’s focus is on neurology and mental health rehabilitation and therapy. We have also created a range of interventions for pain, mental health, lifestyle and disablement conditions.
While our diagnostic approach and internal treatments are allopathic, we also rely on traditional healing therapies to restore the equilibrium of your brain and mind interface. Buddhi Clinic’s seamlessly integrated approach offers 14 non-pharmacological treatment modalities that are an amalgamation of modern science and ancient wisdom.
We offer treatment programmes for each condition customised for children, adults and the elderly. These include: Ayurveda, Acupuncture, Acupressure, Naturopathy- water, mud, aroma and magnet treatments; Reflexology and Yoga; and Rehabilitation therapies – speech, neurodevelopmental, physiotherapy and a range of specialized psychological therapies. We have also curated treatment combinations for Psychology – CBT, CRT, Behavioural, JPMR, ERP, EMDR; and Neuromodulation or brain stimulation (a full house of treatments).
Empowering the Patient Based on the “McDonald’s Model”
One of the guiding principles behind founding Buddhi is respecting and understanding patient preferences and engaging patients in shared decision-making. Towards this end, we perceive our startup to be the McDonald’s of “Brain and Mind Care and Rehabilitation”.
Similar to how a customer can curate his meal in a McDonald’s outlet, Buddhi Clinic, too, offers patients the choice to curate integrated treatment programmes tailored to their specific needs. This is called the “choice model” and is better suited for mild impairment and chronic or progressive health conditions. In such situations, we give patients the choice and flexibility to select a combination of modern and ancient interventions rather than rely on a single medical treatment, procedure and therapy. It is our belief that for best treatment outcomes, the patient should be in control of his own decisions regarding his healthcare options.
That said, our team also draws up a “prescription model” when the patient suffers from a chronic condition and requires continuous restoration and rehabilitation.
Crucially, at Buddhi Clinic, we adopt a holistic approach to healing our patients and focus on their overall wellness and recovery that goes beyond cure. We think different—not just about illness or disablement but also about ability and enablement.
Research and Innovation Led Approach
Nothing fulfils me more than making sustained efforts to give our patients a better quality of life. Our patient-focused approach includes continuously monitoring their progress and offering them quality pre-treatment, mid-treatment and end-of-treatment assessments.
Over the years, we have delivered quality healthcare to over 10,000 patients who have received an excess of 1,00,000 interventions. Our success stories that cover conditions such as autism, epilepsy, depression, Parkinson’s disease and dementia, among others, are documented as detailed case studies in ‘Buddhi Books’. The books are aimed at fostering the spirit of research and continuous learning to enable children, adults and elders achieve a better quality of daily life.
Buddhi Clinic also endeavors to offer innovative products and services to enhance the integrated approach to long-term brain and mind care. For instance, we use Transcranial Magnetic Stimulation (TMS) to treat neurological and psychiatric disorders. Transcranial Direct Current Stimulation (tDCS) and transcutaneous auricular Vagus Nerve Stimulation (taVNS) are also the Neuromodulation innovations we bring in. While the former two, rTMS and tDCS stimulate specific brain pathways for specific conditions and outcomes, the latter tAVNS stimulates the auricular (ear lobe) branch of the vagus nerve (ABVN), an easily accessible target that innervates the human autonomic nervous system. Like this, there are other innovations in the pipeline that we hope will lead to paradigm disruption in this space.
Building a Service-Oriented Approach
In order to create a healing environment based on holistic principles, we aim to continue to provide personalised and meaningful patient experiences at competitive rates. Since today’s patients have greater discernment, patient satisfaction is paramount to us. Our service-oriented approach helps us deliver, on an average, 10-20% more therapy to each paying client, apart from serving the disadvantaged at low cost or free of cost.
In the coming years, it is our goal to collaborate with doctors and diverse talents in the healthcare sector to serve populations beyond Chennai and India. Our objective is to demonstrate our capability as pioneers and leaders in integrated care with a brain and mind focus.
One of my key learnings as a healthcare entrepreneur has been that it’s not enough to achieve a robust bottom line growth. It is equally important to sustain it by creating impact at scale through a committed patient-focused approach.