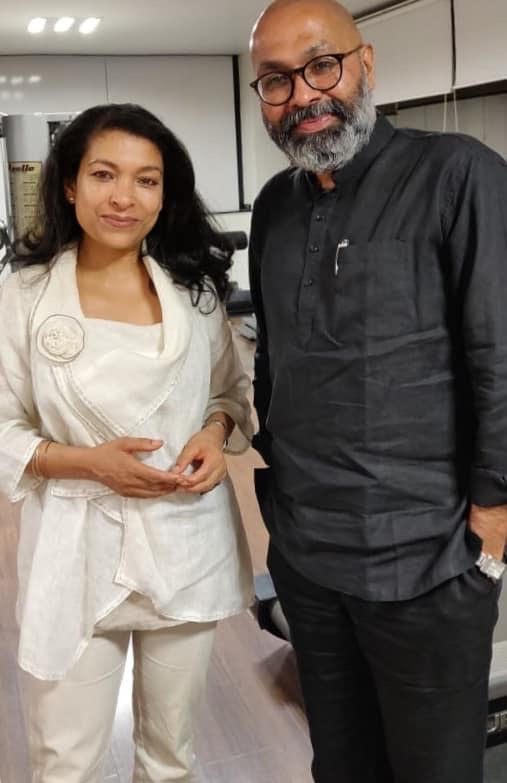
A conversation between Dr. Sheela Nambiar MD, Obgyn – (SN) and Dr. Ennapadam S Krishnamoorthy – (ESK), Behavioural Neurologist & Neuropsychiatrist.
SN – Welcome to you all. We are happy to be here to discuss this important topic of depression. Dr Ennapadam Krishnamoorthy is a Neuropsychiatrist in Chennai and Behavioural neurologist. He is the Founder of the Buddhi Clinic chain which offers complementary and alternative medicine, in addition to, standard neurological & psychiatric care and psychotherapy solutions.
SN – Why would you say the disease of depression has become an epidemic of the 21st century? Is it something that we are calling out more or are people more depressed than say, 20 years ago?
ESK –We understand today that depression is one of the most common medical problems worldwide, a cause of dysfunction and debilitation. At one end it is just a feeling most of us will experience at some point in our lives, due to life circumstances or, a loss. Sometimes it might last for a short spell. At other times it may last for a longer period of time and affect our lives. That is when it becomes a disability.
Let’s say, I break a leg – it is a very apparent disability. But, when I am depressed, no one else may know what I am going through, because it is so personal and internal that it cannot be communicated to others. It is a transient feeling but that which disables an individual and prevents her/ him from having a normal life.
A meta-analysis from BMJ looking at how depression has progressed actually shows that the rates have dropped from 36% to 24% in patient clinics. The paper also says you are more likely to be depressed in your 30s and 40s and then late in your life. So it’s a “U” curve. So I’m not sure if it is indeed more common than before.
SN – So what is the difference between feeling low and having a clinical depression?
ESK – The difference is in the severity. Is it significant enough to need attention? How long has this gone on? The duration can be as less as two weeks. But the most important thing to ask oneself is – ‘is it preventing me from having a normal life?’ If it is, one needs to pay attention to it.
SN – What is really interesting to me is that everybody has problems. I don’t think anyone gets away without problems. How is it that some people are able to withstand them and not become depressed, whereas others having similar issues get depressed?
ESK – So in your introduction you used the term “bio-psycho-social”. The Bio part of it is how each of us is wired. This is a combination of genetics, early upbringing and the like. This is when the brain develops. Your ‘Bio’ is influenced by your genes, by the chemistry in your brain, certain inflammations like the antibody syndrome when your body is attacked by something, the body responds by creating antibodies but which then turns against your own body’s cells. There are metabolic factors that cause depression. These could be hypothyroidism, low B12, D3, having diabetes, and certain skin conditions like atopic dermatitis. We, then, come to Psyche which is your temperament. Certain temperamental patterns, like worriers, obessesive anxious people may be more prone to depression. There are Social-environmental factors which include parenting, family, outside influences etc
So, the question “why am I getting depressed”? has multiple answers – we all have emotional scars of various kinds, some we may not even remember. We also have nurturing factors that make us stronger. People who are worriers, obsessional, anxious, tend to be more prone to becoming depressed than people who take things in their stride and just move on.
SN –And there is some research on how more creative people tend to be more prone to depression is there not?
ESK – Oh yes. There is a lot of literature on mood swings and creativity. There are a number of examples of poets, artists and people in the creative field who were depressed. That’s also because depression is more of a right-brain than a left-brain phenomenon. Having said that, there are forms of depression that are left-brain too. There is a social aspect to depression, one interesting statistic is that you are seven times more likely to have a mental health problem in the 6 months after your marriage than in any other time in your life!
But interestingly there is another counter-statistic is that one of the things that makes sure that you have a good outcome from a mental health problem is being married.
ESK – Women are twice as likely to experience depression in their lives than men are. Due perhaps to all the life events they go through and the hormonal changes.
SN – Hormonal fluxes can be quite drastic from menarche, to pregnancy and delivery to menopause. These events do influence a woman’s mood. Would you say that social support also plays a role in depression?
ESK – Absolutely. Both in protecting you against depression and in helping you overcome it. Having a good social support system, work and employment, activities you resonate with and a healthy financial status.
SN – I deal mainly with women being a gynaecologist. I find that women, once they cross the age of 40 or so, find themselves wondering what else to do, now that their children are independent Once they are given some support, they make a change that they perhaps could not attempt in their 20s and 30s. It may be maturity or that after a point they no longer want to please society, norms or the people around them all the time. One of the triggers for this change is that they start to feel depressed. Have you come across situations like this?
ESK – Absolutely! Menopause/Perimenopause also plays a role. Mood, memory etc. are affected around this time. Apart from life circumstances, there are biological changes that are happening so symptoms of depression etc. can set in.
SN – What do you have to say about this concept of depression being connected to ‘weakness’ and the stigma behind it? Does this hold back people from coming forward to get help? In fact, even family members may brush it off saying, “you need to get over it”.
ESK – That is the most common thing we say, “pull yourself together’. But they cannot! That is why one needs to understand that it is a disability. If one were paralyzed, one would not say “get up and walk”. There is, also, a burden of expectation we all place on ourselves. The expectation – to be normal and fulfil our obligations. When you are depressed, however, these obligations may seem big. Getting better, just like with a paralysis, is a slow process.
SN – Can you tell us the different symptoms experienced by a depressed person? Do different personalities express depression differently?
ESK – Children and elders express depression differently. A child might be irritable, agitated or angry. Elders might also show similar signs. Though they are both likely to be depressed. In adults, it can be expressed as low moods, or
” Anhedonia” which is the inability to feel pleasure in things you would normally find in, “Hedonism”- to seek pleasure mindlessly, or “Alexithymia” which is the difficulty in verbalizing an emotion.
Language has an interesting connection with depression. There is no word for depression in Tamil for instance. There is no word to say I am depressed in Tamil. You only express things like ‘the mind is tired”.
There are linguistic barriers to expressing depression. Our culture does not encourage you to express your emotions like Western cultures do. Most of us would not for instance, go on the Oprah Winfrey show and talk about our glorious or miserable lives! This is because our culture does not encourage us to express our emotions. People often use ‘as if” terms to talk about emotions rather than talk about their emotions directly. In a number of Indian and other native languages also lack words for certain emotions. Friends from Africa tell me they don’t have a word for depression.
SN – Coming to the treatment of depression, can you tell us something about anti-depressant drugs?
ESK – Anti-depressants have had some bad press. But they have a unique mechanism of action. We used to think they correct the chemical imbalance in the brain and that is what relieves symptoms depression. We now know that some of these drugs actually help to grow new neurons. They have a neuro-protective effect. This may be why they take a long time to produce relief from symptoms. Antidepressants take a long time – 6 weeks to 3/6 months. The most common reason for ineffectiveness of treatment is non-compliance to treatment. The second is the failure to try a drug at an adequate dosage for an adequate period of time. So, often, if 3 months later you don’t feel better, you may change your doctor, your drugs etc.
All drugs have side effects, of course. I think a patient should try anti-depressants under the guidance of a good doctor before they give up. In my experience, most people give up the treatment too easily. It requires a therapeutic alliance between patient and doctor.
SN – Can a patient go off the drugs completely at some stage?
ESK –You cannot stop them suddenly, they need to be withdrawn slowly and gently. Typically, the drug needs to be taken for at least 6-9 months.
SN – Have you come across many patients who complete the course of drugs and do well?
ESK – Depression is one condition where you can actually say you are “cured”. The chances of cure become better when besides taking medication you do other things like psychotherapy. Psychotherapy helps you understand the roots of your depression. Where is it coming from? It reflects the gap between expectation and reality. So, it is important to engage in good therapy and use this opportunity to understand oneself. Good psychotherapy will help you prevent further episodes as well.
SN – So Cognitive Behavioural Therapy would be one such form of Psychotherapy?
ESK – Yes, absolutely
SN – Talking about prevention and lifestyle management of depression, I would like to add about why exercise is so important for the management of depression. Exercise does produce endorphins; it makes you feel better and puts you in a better frame of mind. Diet is also of utmost importance. The gut produces as much if not more serotonins than the brain. The microbiome in the gut is responsible for much of your mood. If you do not feed the gut with the right kind of food, the microbiome in the gut is altered. It has been shown that people with very poor eating habits – highly processed food, sugar and so on have altered microbiome and are more prone to depression. Something as simple as a change in your diet and exercising on a regular basis can be a support system to the medication if you need it.
SN – What can you typically expect from a psychotherapist?
ESK – A good therapist is not someone who will tell you what to do. They will not advice you what to do. Instead a good therapist will show you a mirror to yourself. She/he will be able to help you understand your emotions and verbalize them. A therapist is a professional, and has no prejudices. All the solutions are within us. We may not see them. So, we may need the help of a good therapist.
SN – Is depression genetic?
ESK – Yes, when the Human genome project was underway a number of single gene disorders were discoved. Certain disorders of brain and mind also got unlocked. General thumb rule is that 10% of people have a genetic form of neurological or mental health condition.
Talking of psychotherapy – Everyone may not be suitable for psychotherapy. You cannot offer psychotherapy in all stages of depression. You may need to work with some people in other ways.
SN – Lets open the floor for questions
Question – When you are looking after family member with depression, how do you deal with them when they don’t comply with medication? What is the right approach when they refuse to take responsibility?
ESK – The role of the family and in having someone empathetic is important. Sometimes, when the patient refuses to come to the hospital we, at Buddhi Clinic will send someone to their home to try and engage with them.
Using holistic care like Yoga and Ayurveda, (which is offered at Buddhi clinic), we can get them started on a self-care journey.
Then, there are head massages. What a head massage does, which we now understand through research in other areas, is that it probably changes the energy metabolism of the brain.
So, engagement, having the family involved, offering people courses that they truly believe in and are willing to explore have a hugely beneficial effect on the management and better cure of depression. I became interested in these other forms of treatment after I found that often people with mental disorders when they try alternative forms of treatment like yoga etc. they are told to stop all other forms of treatment. So I decided why not offer them everything so they can continue their medication when required and also have the option of other treatment under supervision. We don’t understand the power of what other systems can offer.
A friend of ours who does research on Yoga has shown that after a set of Yoga sessions which are aimed at improving mood, the brain changes are the same as taking medication.
SN – With reference to this first question it is important to also rule out other disorders isn’t it? It may not be pure depression. It is possible that it may be a combination of mood disorders, psychosis and so on?
ESK – Thank you for pointing that out. It is important to recognize that what seems to be depression may be something else. It could be a disorder of the brain or body.
SN – It could be a simple deficiency like a B12 or D3 deficiency.
ESK – Yes or it may be an inflammatory condition of the thyroid for instance. Thyroiditis that is completely treatable.
Question – Is it true that depression can teach you something and it is there for a reason? Can the person be depressed because he needs to withdraw and ponder?
ESK – That’s a very interesting question. If you read the life stories of Ramakrishna Paramahansa, Jiddu Krishnamurthy and others you will find that for many, transformation and realization started with depression. “Pathos” is the word used. That does however, not hold good for everyone.
ESK – One of the things we have not mentioned about depression is the Becks Triad – this is the negative view about the world, the self and the future.CBT is circled around this thought process to identify the thoughts that are making you depressed and work on how you can re-think.Today we also have Transcranial Magnetic Stimulation TMS. For some this works very well. It modulates your brain and makes the chemicals more available. We have this treatment available at Buddhi Clinic. You need 20 sessions of about 30 minutes each. No anaesthesia is required.
Question – What do you advice people who are the caregivers of depressed people?
ESK – It has a profound effect on the family and caregivers. Caregivers go through a lot of stress. An important part of caring is to also extend it to the caregiver. Caregivers go through guilt, blame and remorse. Usually the psychotherapist is the best person to discuss this with. You don’t always have to do something active with a person who is depressed. Just sitting with them, going for a walk with them, listening to music may be sufficient. Just being there sometimes makes all the difference.
Question – What is the relationship between substance abuse and depression and what effect do they have on each other?
ESK- It is a kind of chicken-and-egg story. With some, being depressed may make them turn to substances like alcohol. In others, the alcohol is the problem and leads to depression. So, the drinking and the mood may be cyclical.
Questioner – What about food? Is that also a form of substance abuse?
ESK – There is a lot of association between eating disorders and mood. Anorexia and bulimia are associated with mood disorders. So, eating disorders and mood disorders can co-exist in a number of people. One can influence the other, the treatment of one can cure the other.
SN – There is evidence that obesity is related to depression and vice versa. So, when you are depressed, you reach for food as comfort, gain weight and then you get more depressed. Frankly I think food is as addictive as any other substance (abused), because it is so easily available, acceptable and accessible unlike alcohol and drugs. Especially sugar, not just white sugar but processed food that has added sugar is highly addictive.
SN I would like to thank Dr. Ennapadam S Krishnamoorthy who has been so generous to spare his valuable time to come here and spend this hour with us to discuss depression. It is silent, pervasive and so easy to miss. If you have any doubts about anyone (including yourself) heading down that road, there is no stigma. It is like any other disease. Just as you would not hesitate to go to a doctor to treat gastritis, there should be no stigma associated to going to a psychiatrist.
I hope Dr. ESK has made it clear and that is all the more reason we should pay close attention to it.