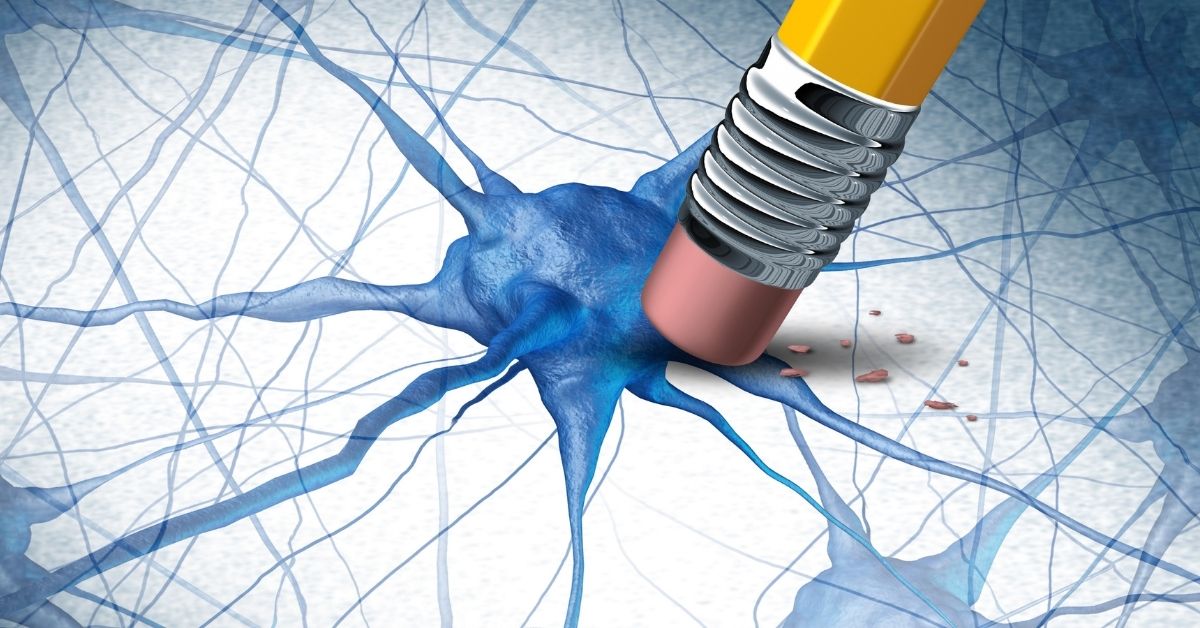
A is a generally healthy and active woman professional of about 48 summers. I know her socially, well, and was curious when she sought an urgent appointment to see me professionally. “I am losing my memory doc”, was A’s first statement as she walked into my office. Probing further I found A was complaining of much more that absent mindedness. Word finding difficulties, struggling with routine skills like driving, becoming disoriented on arriving in a hitherto familiar location, not precisely remembering why she was there anyway, the list seemed endless. “Am I getting Alzheimer’s doc” was her genuine concern, expressed more than once as our interview progressed.
Different Strokes
I asked her about her general health- whether she had any of the four key lifestyle risk factors which predispose to memory loss: Hypertension, Obesity, Lipid (high cholesterol) or Diabetes. While she did not have high blood pressure, blood sugar or cholesterol, she had been overweight until 2 years ago when she went ahead and elected to have bariatric surgery abroad. Following this she has lost considerable weight and had been on a rather severe diet that was recommended for about 18 months after. “I am slowly resuming a normal diet, but the quantities I eat remain small”, said A. On questioning she reported normal thyroid function, no lupus or other such inflammatory condition, both of which can also predispose to memory problems in younger people. Her heart and kidneys had been declared “fit and well” by her physician, during her last master health evaluation. What about your monthly periods, I demurred? “Menopause finally set in doc, about 2 years ago”, said A. When did the memory problems start, I wondered? A thought for a few moments before responding; “about the same time as my periods started tapering off” she responded. A clarified to leading questions that she was not under any significant emotional stress, nor were there any stressful life events in recent times. Indeed, with both children off to college and her husband having come into considerable wealth recently, A felt life could not be better, especially as they now had the time, resources and freedom to travel, something they both enjoyed. I asked her about neurological events or symptoms during her lifetime: head injury, seizures, fainting episodes, strokes, to all of which she replied in the negative.
On physical evaluation A was completely well and there were no signs of concern. On the bedside evaluation of memory and cognition, though, I found A struggled a little with tasks of attention (focus), recent memory (recall) & executive function (ability to perform tasks in sequence), resulting in her working memory being somewhat affected. She did manage to remember and perform most tasks: however, she was a little less efficient and speedy than I expected her to be, considering that she was a smart & efficient professional. The obligatory brain scan (as a measure of safety) was normal, but her blood tests revealed that she was deficient in vitamin B12 (an outcome of her dietary restrictions following bariatric surgery) with elevated homocysteine, a brain chemical that is associated with memory problems. I concluded therefore that A had two reversible causes of memory impairment: vitamin B12 deficiency & menopause.
The Menopause Effect
The World Health Organization defines the perimenopause as the time immediately preceding the menopause, beginning with endocrine, biologic, and clinical changes, and ending a year after the final menstrual period. The Study of Women’s Health Across the Nation (SWAN) published in the American Journal of Epidemiology (2000) showed that of 12425 women aged 45-55 years across sociodemographic categories who participated, between 31 and 44 % of perimenopausal women, endorsed forgetfulness. Overall perimenopausal women were 1.4 times more likely than premenopausal women to be forgetful, this finding not being just due to emotional stress. Indeed, there is considerable research today to show that in the year after the final menstrual period, women do demonstrate deficits in attention, working memory, visual & verbal memory and motor speed. Interestingly, studies like the “Harvard Study of Moods & Cycles” show that in the perimenopausal period, women are twice as likely to be depressed, and while this is not related to negative life events, it is associated with vasomotor symptoms (hot flushes). This links up with the theory that the brain hormone cortisol (which exercises an influence on the reproductive hormones) may be associated with both memory and mood; that higher cortisol levels and/or greater cortisol reactivity may be the biological link between hot flashes, depressive or anxiety symptoms and perimenopausal decrements in memory. Indeed, research has shown that young women have lower reactivity to cortisol than older (perimenopausal) women. This of course brings up the inevitable question, which A asked me “doc, should I be on Hormone Replacement Therapy”? HRT has been both praised and vilified (like many medical procedures) in equal measure. The summary evidence suggests that HRT commenced during the perimenopausal period has the potential to help symptoms of mood, anxiety and perhaps importantly, memory. However, HRT started outside these time periods does not appear to have a similarly beneficial effect, indeed may even be detrimental.
Prevention & Cure
I had identified in A, apart from menopausal transition, a reversible cause of memory impairment, vit B12 deficiency with elevated homocysteine; which has an impact on memory and makes one vulnerable to having strokes. Other reasons why middle aged individuals like A have problems with memory include depression, infections, inflammations and metabolic (including thyroid) problems (all reversible); cancer, strokes & brain tumours (potentially reversible, at least in part); and brain degeneration (non- reversible but can be slowed, partly arrested). It is for this reason that people with memory complaints in middle life like A, need to be thoroughly evaluated for a range of causes. A did go through such an evaluation before we concluded that her problems were due to menopausal transition and B12 deficiency, both of which we proceeded to address. We recommended to her, all those things that can help a person stave off memory loss (and indeed lifestyle disease): a healthy and predictable life, an antioxidant rich diet, adequate rest and sleep; regular aerobic exercise (walking, jogging, gymming); yoga, pilates or tai chi as mind-body interventions; moderation in all that one does, including and especially social consumption of alcohol. Turmeric is today in advanced trials and extra virgin coconut oil in early phase trials as a memory protecting agent. The former is adequately present in Indian diets generally; the latter easy to add, admixed with rice etc. We recommended both to A.
We learnt from her too, as we do from all patients; the links between mood, memory & menopause, preventive health and the importance of holistic evaluation and care. All memory loss is not dementia and women like A in menopausal transition would do well to consider and address that aspect of their health.