When symptoms defy explanation, an interdisciplinary approach works best.
When I first met Mrs. A, the wife of a practising physician, she had been clinically symptomatic for over two years. Her main complaints were an uncontrolled appetite (she was eating every two hours and in large quantities), weight gain (over 10 kilograms), irritable bowels (she was visiting the loo every two hours as well), vague aches and pains, fatigue and excessive sleep. She had consulted an army of specialists of every conceivable description, undergone (often repeatedly) a battery of investigations, no specific abnormalities being identified and consequently no diagnosis having been made.
Each person who saw her had given her a diagnosis: the gastroenterologist called it “irritable bowel syndrome”, the orthopaedic surgeon “fibromyalgia” and psychiatrist “atypical depression”. None of these diagnosis or treatments thereof had resulted in symptom reduction. Mrs. A was thus at her wits end when we met, desperate for a diagnosis and a cure.
Mrs. A is one of many people who suffer from a distinctly peculiar condition: unexplained medical symptoms. Clinical studies have shown that over 30 per cent of people attending out-patient clinics and emergency rooms have medical symptoms without ostensible cause. Indeed, a plethora of examinations and investigations done in these individuals fail to reveal any specific clinical abnormality, or diagnostic entity.
Shuttling between doctors, hospitals and diagnostic facilities, they often remain clueless about the real cause of their symptoms. Over time they develop a cynicism about the healthcare environment and proceed to explore alternative options. Meanwhile, healthcare professionals also become cynical toward such individuals, labelling them “neurotic”, “anxious”, “hysterical” and other potentially disparaging terms.
A famous study by Dr. Eliot Slater — an eminent psychiatrist in the National Hospital for Neurology, Queen Square, London — followed up over a decade, all those diagnosed with “hysteria” in this pre-eminent institution and showed that a very large proportion (about half) went on to develop “real” medical illnesses. The results of that medical study published many years ago, warned physicians about the dangers of writing off unexplained medical symptoms as being “hysterical” or “in the mind”.
A repeat study in the same hospital in the 1990s, under the guidance of Prof. Maria Ron, an eminent neuropsychiatrist, showed that the rate of erroneous labelling as “non-organic” had fallen to about 10 per cent, aided no doubt by advances in medical technology. It must be noted however, that mis-diagnosis as “non-organic” or “in the mind” continues to occur even in pre-eminent medical institutions staffed by experts with access to best medical technology. Having said that, a number of people with unexplained medical symptoms do have “non-organic” causality.
So why do people have unexplained medical symptoms? A proportion, perhaps, have a genuine medical cause or complaint that has remained undetected. Examples include inflammatory, infectious and metabolic conditions, and rare forms of cancer that may take time to manifest their full avatar. A proportion may have true hysteria — deep psychological trauma that is finding its outlet in physical symptomatology with secondary gain being the attention derived thereof.
A proportion may be addicted to the hospital environment — “Munchausen’s” hospital addiction syndrome — leading them to repeatedly seek contact and reassurance from healthcare professionals. A proportion may have health-related anxiety and engage in so called “abnormal illness behaviour”, with their reactions being out of proportion to the symptoms they are experiencing. A proportion may be engaging in conscious malingering, presenting a medical symptom in order to avoid a social problem, for example, an arrest or a court appearance.
In all people with unexplained medical symptoms, the bogey of an “organic” cause that has hitherto gone undetected, needs to be kept in mind. Repeated and detailed history-taking and clinical examinations are necessary, as is a close and empathetic follow up, with neither the physician nor the patient’s family succumbing to the proverbial “crying wolf” syndrome. In patients in whom an organic cause has been excluded beyond reasonable doubt, hysteria, somatisation (multiple physical symptoms without a physical cause), Munchausen’s syndrome, Abnormal Illness Behaviour and malingering may all be considered and form part of a psychological continuum.
What varies across this continuum is the level of conscious awareness, considered low (hence unconscious) in hysteria and somatisation, and high (hence conscious, deliberate and wilful projection of symptoms) in malingering. What varies also is the motive or intent; preference for the hospital environment in Munchausen’s syndrome, avoidance of a social problem in malingering, or indeed the more fuzzy and less easy to diagnose “secondary gain” of hysteria and somatisation. In all these instances, an empathetic approach, with deep understanding of the client’s background (developmental, familial, social, occupational and marital) is necessary, as is a strong therapeutic relationship rooted in mutual respect and trust.
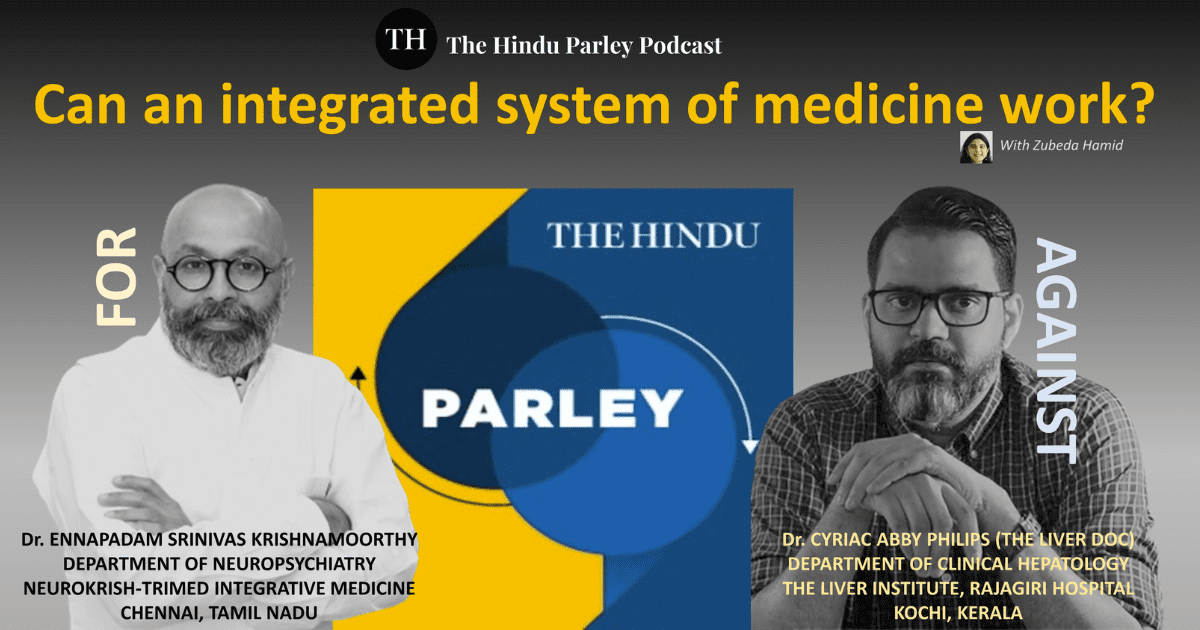
All the above seem a tall order when demanded from a solitary physician doing her/his best with the constraints of time and resources. Patients with unexplained medical symptoms do well when managed by an interdisciplinary team. Such a team usually is lead by an astute clinically focussed physician, supported by nurse practitioners, physical therapists, psychological therapists and counsellors, nutritionists, and other caregiving professionals.
In the emerging space of integrative medicine, physicians from a host of alternative disciplines like Naturopathy & Yoga, Ayurveda, Homeopathy, Acupuncture etc. participate in care delivery. For the person with unexplained medical symptoms interdisciplinary care provides the opportunity to both understand and manage various symptoms, physical and psychological, better. Learning to live with what cannot be cured, maintaining one’s activities of daily living and quality of life often become reasonable and acceptable goals.
Mrs. A was diagnosed by an interdisciplinary team, after a detailed evaluation, to have clinically significant autonomic dysfunction, a difficult to diagnose problem with myriad physical and psychological manifestations. Combined with this was an element of “Abnormal Illness Behaviour”. Her medical management was suitably augmented to address these complaints and she committed herself to a care program that integrated physical, psychological and nutritional therapy with ayurvedic treatments, mud therapy and yoga therapy.
Over a span of three months her symptoms improved considerably: normalization of appetite, regulated bowel movements, improved energy and enhanced activities of daily living and considerably reduced health related anxiety. Her success story underlines the challenges of interpreting unexplained maladies, the crucial role of personalised clinical medicine, the need for interdisciplinary care for chronic medical conditions, and for our intellectual glasnost as a society towards the wealth of clinical wisdom that resides in our ancient medical traditions.
As Hans Berger, the inventor of the Electroencephalogram (EEG) an instrument that studies brain waves, said, “A machine can replace neither common sense nor intelligence”.