Biography
It was six years into retirement, in 2009 when the early signs of mental illness surfaced in a subtle manner in Mr. Jayaram. Where had he kept the house keys? How could he forget to buy the cooking oil from the shop round the corner? He had never missed even one of ten items for routine household purchase that his wife verbally listed to him and so she spared herself the trouble of writing it down. Jayaram brushed aside his occasional memory lapses, and went on to read the day’s news, reclining comfortably in his planter cane-and-wood ‘easy chair’, while his wife brought him fresh south Indian filter coffee, even as the television audio sounded the Suprabhatham, the gentle daily chant to wake up the Lord of the Seven Hills.
The wife began to register concern as the memory lapses occurred more frequently. Jayaram appeared agitated at times as if he was experiencing an inner turmoil. Soon he showed signs of social withdrawal.
Exploring the Condition
When the family physician was approached for a routine check up of his hypertensive and diabetic status, for which he was on regular medication for several years, the wife shared her concerns with the doctor. A specialist consultation was advised, but at the very heel of the neurological consultation, Jayaram had lost his way home along his oft trodden path and had to be escorted to his house by tense family members and neighbours. A repeat of this behaviour resulted in GPS tagging and going out on his own became a taboo. A diagnosis of Alzheimer’s Disease was made and T2 Hyperintensities (with his history of long-term diabetes and hypertension) on MRI brain suggested an added vascular element to the dementia.
Following a successful career in a position of authority in Central Government, Jayaram had returned to his hometown near Chennai with his wife to settle to a peaceful retired life. His son and daughter having been married a couple of years earlier, had settled abroad with their respective families. They visited the parents once a year. Jayaram and his wife travelled to USA to be with the children and grandchildren for a few months, as was the practice with many Indian parents with children abroad. Life seemed to offer the best of both worlds. However, this state of well-being was not to last forever.
In early 2015, Jayaram’s condition took a marked downhill course. He developed global insomnia, decreasing appetite, weight loss, and refusal to extend his cooperation in simple activities of daily living, leaving the wife, the principal caregiver, in a desperate state and with increasing inability to cope with the situation. She was in a near ‘burn-out’ phase and that is what brought her to the doors of TriMed-Neurokrish. He was bed bound, with double incontinence, expressive aphasia (inability to express language through speech or writing), and probable unexpressed pain and discomfort, resultant behavioural and psychological dysfunction. He became stubborn, refusing to follow any instruction. However, formal psychological testing revealed that he had retained several of his cognitive abilities. Repeated and staggered assessments had to be carried out, deriving maximum diagnostic leads during the lucid phases of orientation and patient co-operation.
Our Healing Approach
From the start, the patient management by our team had to be home-care based, since transporting him to the clinic would prove to be a great ordeal all round and would cause exacerbation of behavioural symptoms. A global assessment of the patient was the first step. Jayaram was clearly heading towards Stage 3 Dementia, in the absence of stimulation and positive hand-holding.
The patient was already on multiple drugs for Dementia, Behavioural and Psychological Symptoms of Dememtia (BPSD) and comorbid conditions, prescribed by his regular Neurologist and Diabetologist over the years. He was on Escitalopam 10 mg – 0-0-1 (a mood elevator), along with Tab.Donamem 10 mg – 0-0-1 (a combination drug of Donapezil and Memantine and specific for dementia), Tab.Oleanz 2.5 mg – 0-0-1, Olanzipine (an antipsychotic), Tab.Ativan 1 mg – 1/2-0-1, Lorazepam (for a tranquillising effect) and follow up with a Diabetologist and General Physician, who had prescribed regular Tab.Glyciphage 1-0-1, Tab.Telista (Telmisartan) 40mg – 1-0-0, Tab.Ecosprin 150 mg – 0-0-1 and Tab.Tonact TG (Atorvastatin) 0-0-1 towards control of diabetes and hypertension and blood thinning and cholesterol-lowering actions, respectively.
The team decision was to cash in on the patient’s cognitive reserve after reshuffling the regular medicine regimen and introducing add-on medication to tame the BPS. In short, the focus was on pharmacotherapy to control the BPS, and cognitive therapy to encourage re-establishing basal activities of daily living to start with. He was treated with Dicorate ER 1 g a day and Tab. Escitalopam 10 mg was stepped up to 1-0-1, in addition to Donamem and his other regular medication. The physiotherapist encouraged gait training in a graded manner till the patient was able to walk around the house with support. With this the BPSD symptoms decreased. Remission or reduction of BPSD is known to produce remarkable improvement in the functional and even cognitive abilities of the patient, which it did in the case of Jayaram. He became more responsive in interpersonal relations, responded to questions, showed some improvement in memory in terms of alphabets, numbers and was able to indulge in meaningful physical activities like throwing a ball.
Glycemic control was one of the foremost challenges at this point, with an erratic dietary pattern, at the patient’s bidding, often ending with poor intake followed by binging on carbohydrates and sweets of his preference. His regular diabetologist reviewed his diabetic status. Jayaam needed a short period of hospitalization as his blood sugar levels were high. On Tab.Galvus Met 50/500 – 1-0-1 and Tab.Diamicron 80 mg 1/2-0-0, the most recent prescription, good control of blood sugar levels and hypertension was established. A lipids review showed a high level of triglycerides and cholesterol. With titration of the drug dosage during his period in hospital, his medication was lowered subsequently to Escitalopram 10 mg – 0-0-1 and Tab.Dicorate to 750 mg – 0-0-1, and the significant control of the BPS remained. However, the occasional lack of overnight sleep would bring on the screaming, which started as a whimper, built up to a crescendo, staying high-pitched for prolonged stretches into the morning hours.
Meanwhile Jayaram developed an intermittent headache, which he indicated by constantly holding his head with his hands, and tucked between his folded knees. As BPS can increase with pain or other discomfort, a detailed investigation for headache was done and diagnosed to be an exacerbation of the migraine which was recorded in his past history. He was treated with Tab.Sibelium 5 mg, 1 at bedtime which effectively controlled the headache.
Initial hand-holding of the spouse to reduce caregiver fatigue and hopelessness was an essential part of the treatment plan, as much to safeguard her health status as to encourage her active participation in the management of the patient. She had meanwhile learnt to cope with his illness, having reached the acceptance stage. However, episodic exacerbation of caregiver distress was inevitable in spite of formal caregivers employed.
“Initial hand-holding of the spouse to reduce caregiver fatigue and hopelessness was an essential part of the treatment plan…”
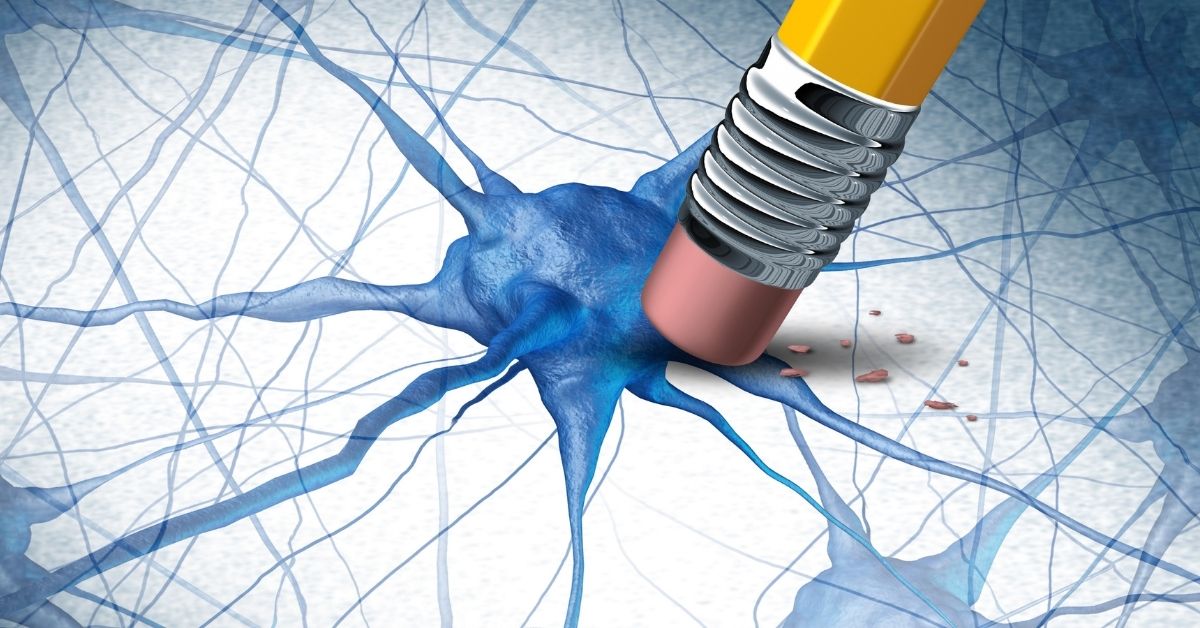
Dementia
Behavioral and Psychological Symptoms of Dementia (BPSD), represent a heterogeneous group of non-cognitive symptoms and behaviors which occur in subjects with dementia. BPSD include agitation, aberrant motor behavior, anxiety, elation, irritability, depression, apathy, disinhibition, delusions, hallucinations, and sleep or appetite changes. BPSD constitute a major component of the dementia syndrome irrespective of its subtype and it has been estimated that it affects up to 90% of all dementia subjects over the course of their illness (Lyketsos, 2015). BPSD is probably the result of a complex interplay of psychological, social, and biological factors. Recent studies have emphasized the role of neurochemical, neuropathological, and genetic factors underlying the clinical manifestations of BPSD.
BPSD also have a profound physical and psychological impact on both the formal and informal caregivers. A considerable part of caregiver distress relates directly to the manifestation of BPSD. Caregiver burden refers to the presence of problems, difficulties or adverse events which affect the life of significant other(s) of the patient (Platt, S., 1985). It is the extent to which caregivers perceive their emotional, physical health, social life, and financial status to be affected as a result of caregiving (Zarit et al., 1986). A qualitative quote from an Indian study reflects the Indian ethos and culture of caring for a near relative: ‘‘Why are you using the word ‘Burden’? My father is not a burden to me. It is my duty to care for my parent and doing so makes me a little tired but gives me great satisfaction.” (R.D. Pattanayak, 2010). Regarding BPSD, these symptoms are stressful for the co-resident caregivers, who lack support and guidance from the health care delivery system which service is poor in developing nations (Shaji K.S., 2009). Prince observes “Our findings underline the global impact of caring for a person with dementia and support the need for scaling up carer support, education and training.. Carer benefits, disability benefits for people with dementia and respite care should all be considered” (Prince, M., 2012).
References
- Helen C. Kales , Laura N. Gitlin, Constantine G. Lyketsos Assessment and management of behavioral and psychological symptoms of dementia, State of the Art Review BMJ 2015;350:h369
- Platt, S., 1985. Measuring the burden of psychiatric illness on the family: an evaluation of some rating scales. Psychol. Med. 15, 383–393. Zarit, S.H., Todd, P.A., Zarit, J.M., 1986. Subjective burden of husbands and wives as caregivers: a longitudinal study. Gerontologist 26, 260–270
- R.D. Pattanayak , R. Jena , M. Tripathi , S.K. Khandelwal , Asian Journal of Psychiatry 3 (2010) 112–116 Shaji, K.S., George, R.K., Prince, M.J., Jacob, K.S., 2009. Behavioral symptoms and caregiver burden in dementia. Indian J. Psychiatry 51, 45–49.
- Prince M., Brodaty H., Uwakwe R., Acosta D., Ferri C.P., Guerra M., Huang Y., Jacob K.S., Llibre Rodriguez J.J., Salas A., Sosa A.L., Williams J.D., Jotheeswaran A.T.,Liu Z. Strain and its correlates among carers of people with dementia in low-income and middle-income countries. A 10/66 Dementia Research Group population-based survey Int J Geriatr Psychiatry. 2012 Jul;27(7):670-82.
Looking Ahead
The merciless progression of the degenerative process cannot be halted or reversed at this stage of medical knowledge. However, reducing the BPSD significantly, encouraging some physical and mental activity in the patient and allowing some calm to prevail is in itself noteworthy.
The spouse’s understanding has changed from vacillating between anger, fear and panic, to one of acceptance and the need for pursuing individual activities to the extent possible within the circumstances. She is in better control of her emotions. She is aware that with progression of the degenerative process, the cognitive, language and motor decline will be steep and that the character of the BPS often can change from one of positive symptoms of aggression, night-wandering to a predomi-nant negative symptom cluster, characterized by apathy. She is thankful for being able to give some quality of life to her husband, and to have achieved some peace of mind and calm, having reposed faith in the treating team and managing reasonably with formal caregivers to share the work.She shudders at the thought of the day’s prior to TriMed-Neurokrish intervention when each day was a nightmare. Knowl-edge is power, and with it, if you have extended your resources-physical, mental, emotional, financial to the utmost, you know you have done your best.