

The day we gave back life through saving his liver – Navins story
Humanity is always greater than the problem Navin at his college, and another picture of him and his mother The first time I met Navin
















Humanity is always greater than the problem Navin at his college, and another picture of him and his mother The first time I met Navin
Evaluating R in some detail, we found he had severe deficits in cognition, with very poor ability to remember any new information. Indeed, he took


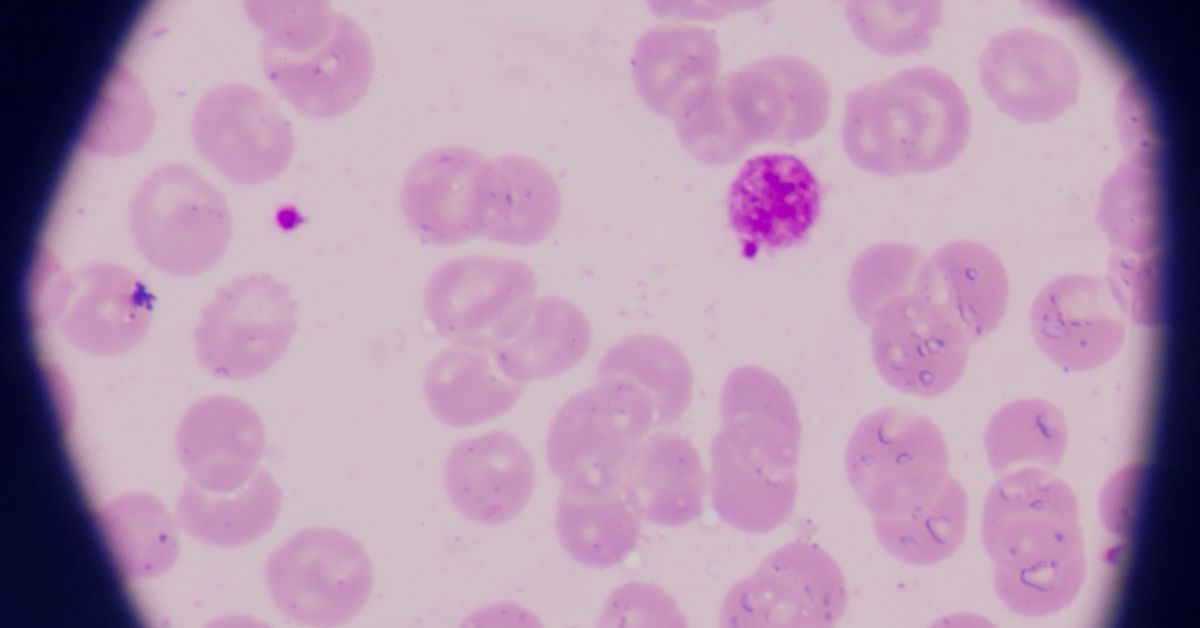
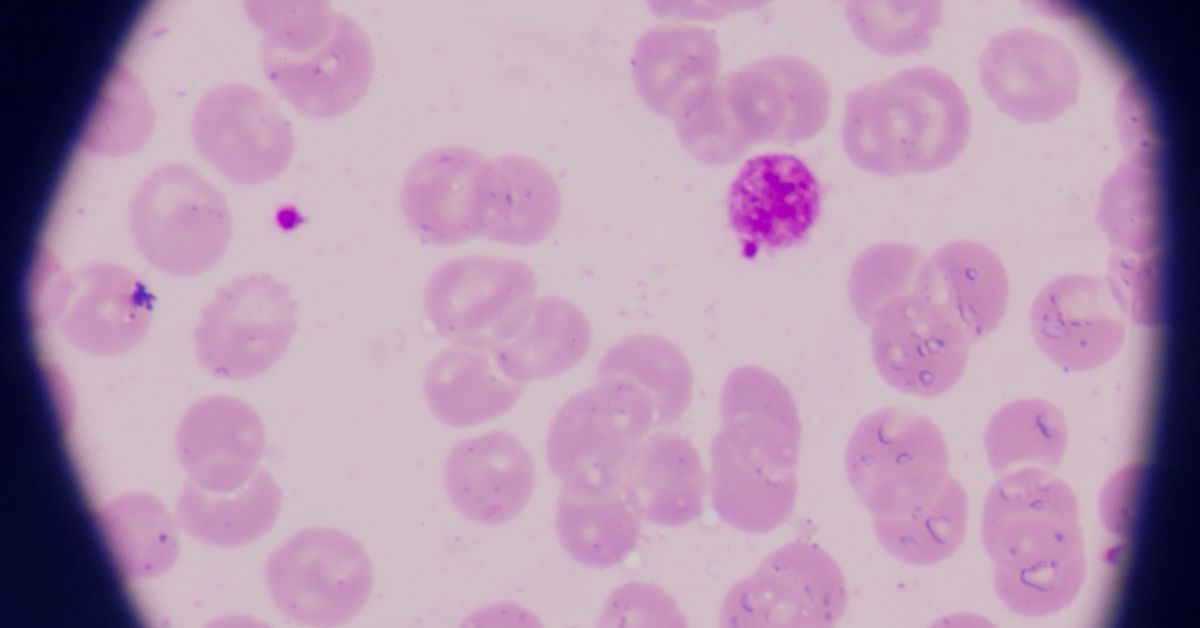
As Hans Berger, the inventor of the Electroencephalogram (EEG) an instrument that studies brain waves, said, “A machine can replace neither common sense nor intelligence”.
We must admit that S’s remarkable progress was made possible by the wonderful therapeutic relationship our team had with his family. From S and his


His aggressiveness which was already on the mend, was helped by the therapy to calm him down further. He was advised to continue the medication


Shanthi co-operated for the therapy. Though there was no significant benefit, her mother was pleased with the procedure and requested a longer period of therapy.


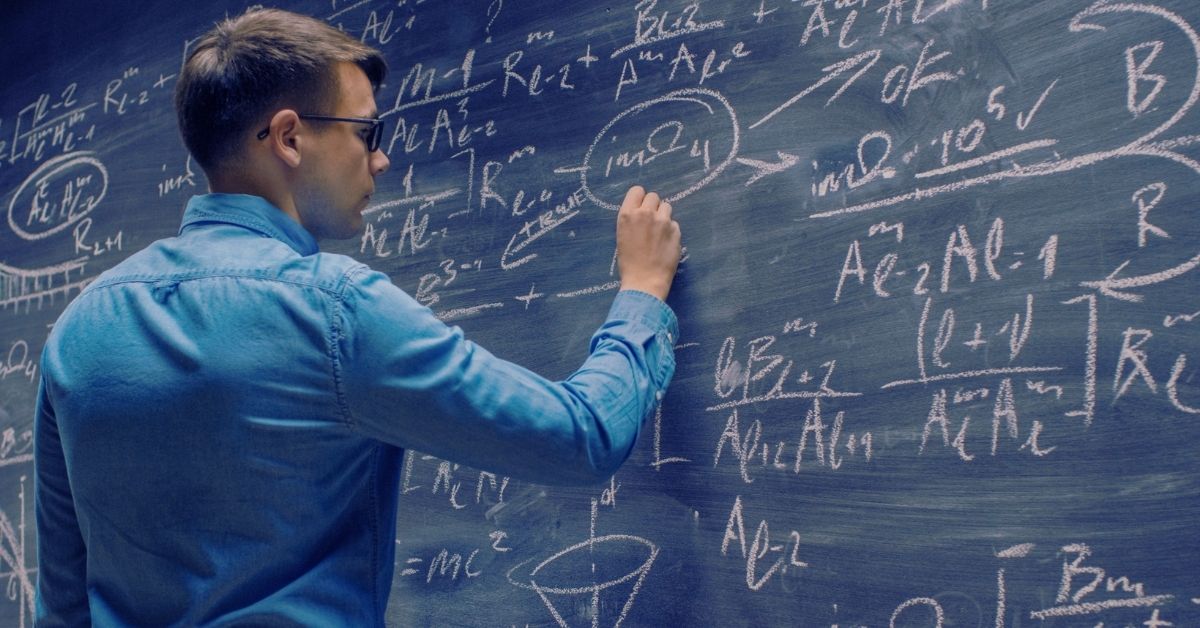
In our advent of going beyond medication, we at Buddhi clinic have an integrative 3M approach that aims at a steady improvement in health for


A disorder that affects adult’s ability to pay attention, control moods and complete tasks, explains the behaviour.


An examination of the Buddha’s views on the mind. Two and half millennia after his time, shows them to be remarkably rational and contemporary.


New Horizons in Elder Care This week, we at Buddhi Clinic inaugurate our new centrally located World Class Resource Hub,representing excellence in brain & mind


Having spent a few decades taking care of elderly family members and several patients , my experiences have changed my perspective of elder care over


Buddhi Clinic’s Brain and Behaviour Dialogue with the legendary Prof. Michael R Trimble of University College, London, curated and presented by Neurokrish The Buddhi Clinic


Mental health is just as important as physical health, especially for children. But how do we help them identify and address mental health issues? Read


The COVID-19 pandemic has brought unprecedented challenges to the mental health of children. But now is the time to look towards a brighter future. Read


Caring for our elderly loved ones can be a rewarding experience, but it can also bring new challenges. Read our blog on how home healthcare
Embracing technology can have a positive impact on children’s lives, but it’s important to strike a balance. Read our blog to explore the effects of


Delve into the 7 Behavioral Changes that can transform the way you feel and cope with daily stressors.


Among all the plans for starting up new, it’s a healthy idea to start your year with the best hopes and practices to elevate your
BUDDHI CLINIC PRIVATE LIMITED © 2023 All rights reserved